Metal on metal hip replacement/ resurfacing
Traditional metal on plastic total hip replacements work well in older less active patients, however there is a higher failure rate in younger more active patients. This is well documented in many publications. This failure rate is mainly due to the plastic socket wearing out and becoming loose. Metal on metal implants were designed to provide a solution to the ‘problem’ of high wear charactoristics seen in young patients with traditional metal on plastic articulations.
Early attempts at designing metal on metal hip replacements had variable success. Most failed, however there were a few that lasted 30-40years.(McKee Farrar/ Ring prosthesis) These implants were made out of Cobalt Chromium alloy.
It was only in the 1980s that Mr Derek McMinn realised that the ‘problem’ with the metal on metal hip replacements was due to a mismatch between the tolerances of machining the implants. Modern implant designs can be produced very accurately so that the socket and head are perfectly matched. This has almost eliminated the phenomenon of cold welding between the head and the socket.
It has been documented for many years that patients with metal on metal implants have higher blood levels of metal ions than patients without. There has been no link identified between cancer and metal ion levels. We do know that metal ions cross the placenta and Cobalt ions are excreted via the kidneys, so kidney function should be assessed before replacement.
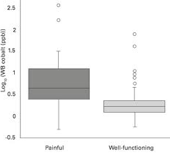
All metal on metal implants have a run in period of the first 6-9 months. During this time the metal ion levels are high and they then settle down in well functioning implants.
Hip resurfacing was first performed in the 1990s in a controlled way by Mr McMinn and specialist trained surgeons. It was very successful and conferred the advantages of a reduced dislocation risk, increased activity level and bone conservation. The modular hip resurfacing head was later released that allowed surgeons use a large hip resurfacing femoral head on a hip replacement stem to reduce dislocation rates. In the last few years other companies have released copy hip resurfacing implants with subtle design changes that have led to a significantly increased failure rate.
Recent investigations have highlighted a number of patients who have persistently elevated metal ion levels in their blood. This has been associated with early failure of the implants and potentially significant tissue damage. Patients with symptoms and high levels require revision surgery.
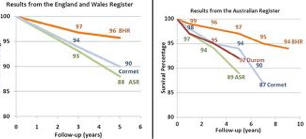
Hip resurfacing using an appropriate implant in a large active male under the age of 55 with osteo-arthritis is a good operation. The reported failure rate at 7 years in the National Joint Registry is 11%. Considering the activity level and demands placed on these implants, this is better than a traditional hip replacement.
The major concerns are with the ASR implant and any modular hip resurfacing head on a hip replacement stem. Other concerns are smaller size implants, female patients and poorly positioned implant components.
The metal ions can be produced from the joint bearing surface itself (especially if poorly positioned) and from the joint between the resurfacing head and hip replacement stem (trunionosis). There are implant centres in the UK that analyse any revised hip replacements/ resurfacings to determine the mode of failure/ wear. This research has highlighted a potential problem with all larger bearing hip replacements where the head joins onto the hip replacement stem. This is currently being investigated and highlights the importance of the United Kingdom having an accurate National Joint Register.

What is the significance of metal ion levels?